Magnetic Resonance Imaging (MRI) is a powerful way of looking inside the human body. MRI is the best available method of looking at the brain, as we are able to see a very high level of detail that can’t be seen on CT scan. Because the MRI takes such compelling images, some people assume that the results will be easy to understand.
However, when most people read the MRI report provided by the radiologist, it seems to have been written in another language.
In some ways this is true – medical terminology contains many Latin and Greek words. Also, there is a lot of incomprehensible technical jargon used routinely to describe the technical aspects of the particular study so that other radiologists know exactly what was done. Radiology reports are written for other medical professionals and not for the general public. That is why the report initially gets sent to the referring doctor who will act as an interpreter to explain to patients or parents the relevance of the findings.
Dedicated children’s hospitals have the optimal set – up for getting the best possible MRI scans in children. One of the biggest problems with MRI is that the patient has to stay very still during the scan because even slight movement distorts the pictures. Just like with photographs, the pictures can end up blurred and uninterpretable. Children’s hospitals have dedicated paediatric anaesthetists who are skilled at administering gentle anaesthesia to keep the patient motionless for the scan. Older children are usually able to have scans without anaesthesia. They may benefit from practicing with a mock MRI scanner and a play therapist so that they are completely comfortable when they have their real scan. Other helpful options are to have music for the child to listen to or DVDs to watch so that the child doesn’t get bored and start fidgeting during the scan. On the whole, children cope very well with MRI, unlike many adults who feel claustrophobic and cannot have a scan without a dose of Valium!
Another consideration is that babies’ brains are not merely smaller versions of adults’ brains but are different in terms of grey and white matter maturity and appearance. This means that a “one sequence fits all” approach will not result in an optimal MRI scan. At paediatric centers, much time is spent changing parameters and technical factors so that the scan will be the best possible for age and size. Even scan planes are different between children and adults. In adults, the axial plane is tilted forwards in order to look for Alzheimer’s changes in the temporal lobes. This plane makes it difficult to evaluate paediatric temporal lobes for cortical malformations.
Advanced imaging techniques such as tractography are rarely used outside of the academic hospital/ research environment and need certain sequences that are not routinely performed in everyday practice.
A radiology report is often organized into 6 sections:
- Type of exam: MRI brain
- Clinical information: this is the history that is supplied by the referring doctor to the radiologist.
- Technique: in the case of MRI this will be a description of the sequences
- Comparison: this is where the radiologist states whether he/she has looked at any previous MRI scans that have been done. It is very helpful to see old scans in order to know whether things have changed.
- Results/Report/Findings: This is the longest part of the report where the radiologist discusses each relevant piece of anatomy and observes whether it is normal or abnormal. In the case of young babies and children, the focus is often on normal development.
- Conclusion: This is a summary of the important findings. If possible a unifying diagnosis will be made. In the case of brain malformations, there are many different combinations of abnormalities; so the summary will likely consist of a list of abnormalities.
You might have come across some of these descriptive terms that are routinely used in MRI reports:
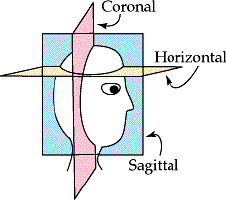
Coronal– this is a slice orientation that looks at the brain as if the person is looking straight at you face to face. This gives a mirror image so their left side is on your right and vice versa.- Axial– (horizontal)-this slice orientation views the brain as if you are looking at it from the feet up to the top of the head with the person lying on their back. Again, their left side will be on your right side.
- Sagittal– this slice orientation views the brain from the side. You would likely have seen your child’s midline sagittal scan, as this is a good way of looking at the corpus callosum in its entirety.
- Sequence– A sequence sets the MRI scan to certain parameters, and collects information under those parameters. Basic sequences are T1 weighted and T2 weighted but there are many different sequences to look at different structures and behaviour of different tissues.
- Hyperintensity/hypointensity – MRI images are presented in grey scale like a black – and- white TV. Pixels range in colour from white to black with many shades of gray in between. White or lighter grey shades are said to have increased signal intensity (hyperintense). Black or darker regions are hypointense. In the brain, grey matter and white matter have different signal intensities that vary with age.
- Artefacts – Distortions seen on the pictures that are caused by motion, metal or scanner issues are called “artefacts”. Even normal body movements such as
breathing, heart beating or swallowing can cause distortions of nearby structures. Artefacts can also be caused by metal such as braces on teeth – this causes a “blackout” over the face and the front of the brain.
These are some terms that you might have come across as part of the ACC diagnosis.
Unfortunately, everything won’t be covered but I hope that these explanations are useful.
- Agenesis means non – formation or absence. This may be complete or partial.
- Dysplasia means that a structure is incorrectly formed or malformed so that it has abnormal components or appearance (other similar words – dysgenesis
/dysmorphic).
- Hypoplasia means that a structure is developmentally too small or too thin. This is different from “atrophy” which means that a structure started off normal in size and has shrunk over time.
- Corpus callosum: the largest white matter tract in the brain connecting the left and right hemispheres.
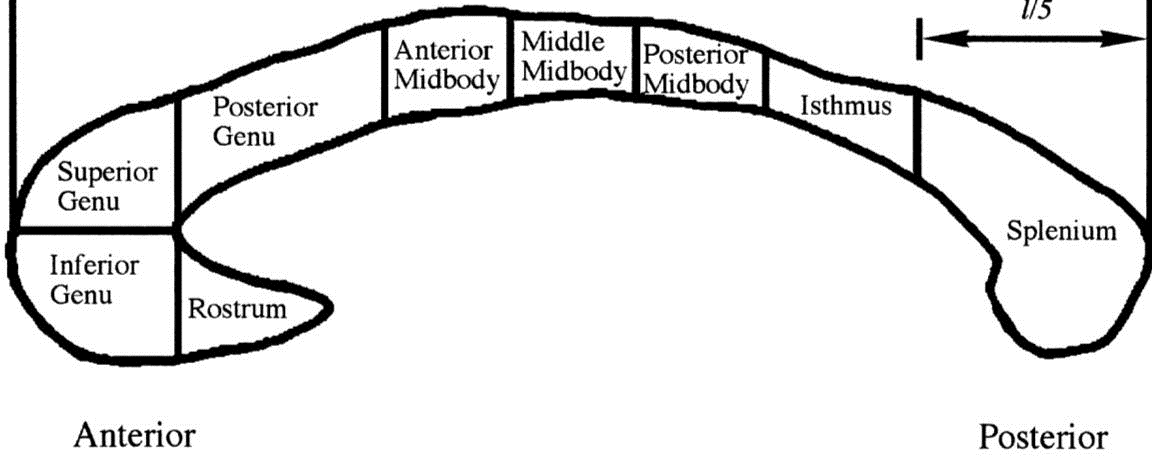
Robin Highley et al. Brain 1999;122:99-110
- Rostrum– front bit (tucked under)
- Genu – the curved bend in the front that looks like a C
- Body – the majority of the CC that runs from front to back
- Isthmus – the thinnest part of the CC
- Splenium – the rounded bulge at the back that is usually thicker than the other components.
- Anterior – front
- Posterior – back
- Colpocephaly – enlargement of the back of the lateral ventricles classically associated with ACC. The ventricles are the spaces within the brain that produce the fluid (CSF) that bathes the brain and spinal cord.
- Cyst – this is a thin-walled structure that contains fluid (a bit like a balloon full of water). Cysts can range in size and number. Sometimes big cysts press on the structures next to them and can cause pressure problems. In these cases, a neurosurgeon might operate to drain or shunt the cyst. In ACC, the cysts are often in the middle between the left and right sides of the brain (interhemispheric).
- Probst bundles are bundles of white matter fibers that are lined up longitudinally along the inside of the two cerebral hemispheres. They are white matter tracts that should have crossed over as part of the corpus callosum to connect to the other side.
It is important to know that a radiology report reflects the radiologist’s opinion about the pictures. As with all subjects, opinions may differ. This doesn’t necessarily mean that one person is right and another wrong; it is a matter of interpretation. Most MRIs in the community are performed on adults who have very different medical conditions to those of babies and children. General radiologists have a lot of experience in looking at adult problems such as strokes. However, most radiologists have not had much training in the detailed interpretation of the subtleties of brain malformations in babies and children.
In the ideal world, all children would be scanned in paediatric hospitals, but in reality there are many reasons why this may not happen. Remember that it is always possible for you or your doctor to send your child’s scan for a second opinion from a more specialized paediatric radiologist or neuroradiologist.
Finally, there is an old radiology saying: “treat the patient not the X ray” (MRI in this case). Each child is an individual and no two individuals are the same even if the MRI reports seem similar. It is not possible to predict how a child will be in the future from the pictures alone. In children with ACC, the MRI is just one small piece of a complex jigsaw puzzle that helps to describe each unique and special individual.
Article by Associate Prof Simone Mandelstam from RCH
